Dr. Demerjian has taken over 2000 hours of postgraduate education courses, in the area of TMJ, Craniofacial Pain, Sleep Disorders and Orthodontics. He is knowledgeable in neuro-anatomy, pain patterns, trigger points, the trigeminal branch/nerve and how it correlates to neurologic disorders. In 2014, he has joined Fontana Kaiser and worked as Project Scientist for the Department of Oral Biology in the UCLA School of Dentistry from from 2014-2018.
Since 2004, he has limited his practice to the treatment of TMJ Disorders, Headaches, Facial Pain, Sleep Apnea, Movement Disorders and Orthodontics. Along with two busy practices, Dr. Demerjian also lectures on topics in Temporomandibular Joint Disorders and its correlates on neurologic disorders.
Dr. Demerjian currently treats adolescents and adults with tmj/mpd-mayofascial pain disorders using custom fabricated orthotic appliances, myriad of therapeutic techniques and orthodontics. His sleep-disordered breathing treatments utilize using multiple dental sleep appliances and therapeutic techniques. He also treats patients suffering from neurologic disorderswith dental management of the disorder through his TMJ treatments. He has published several articles and research papers including how the trigeminal system correlates to neurologic disorders.
Bonita High School, La Verne, California 1980-1984
University of La Verne, La Verne, California 1984-1985
Loma Linda University, Loma Linda, California 1985-1987
University of the Pacific School of Dentistry, San Francisco, California 1987-1990
Diplomate, American Board of Craniofacial Dental Sleep Medicine
Diplomate American Board of Craniofacial Pain
Diplomate American Academy of Integrative Pain Management
Diplomate, American Board of Forensic Dentistry
Diplomate American Board of Forensic Examiners
Fellow American Academy of Craniofacial Pain
Fellow International College of Craniomandibular Orthopedics
Registered Polysomnographic Technologist (RPSGT)
Certified Forensic Consultant-American College of Forensic Examiners
Certified - Academy of Laser Dentistry
Master – Electro-Diagnostic Modalities – Bio-Research Associates Inc.
Current Member
Evidence-Based Dentistry Practice Based Research Network
American Academy of Craniofacial Pain
American Academy of Orofacial Pain
American Academy of Dental Sleep Medicine
American Academy of Sleep Medicine
Pomona Valley Medical Center Sleep Panel
American Academy of Advancing Science
American Dental Association
California Dental Association
San Gabriel Valley Dental Society
Full Bright Association- Greater Los Angeles Chapter
Past Member
American Academy of Pain Management
International College of Craniomandibular Orthopedic
International Association of Orthodontics
American Academy of Functional Orthopedics
American Academy of Cosmetic Dentistry
Academy of Laser Dentistry
Upcoming Presentations:
“TMJ Correlation to Neurologic Disorders” Tri-County Dental Society July 2020
Professional Presentations:
“TMJ Correlation to Neurologic Disorders” International Pain Summit 2019, UCLA Meyer & Renee Luskin Conference Center, Los Angeles, CA November 16
"TMJ Disorders Basics for the General Practice and Recent Findings" Dr. Ammar Study Club November 14, 2019
“Correlation of Temporomandibular Joint Disorders to Movement Disorders” Nierman Conference, Orlando Florida October 26, 2019
"TMJ Disorders Basics for the General Practice and Recent Findings" Dr. Abari Orthodontic Study Club, November 7, 2019
“Oral Appliance Therapy” Rancho Dental Society, March 8, 2019
“Temporomandibular Joint Disorders” Yerevan, Armenia July 2, 2018
“TMJ, Chronic Pain and Neurological Disorders” Armenian American Medical Society, Las Vegas, September 30, 2017
“Arthrokinetic reflex of the TMJ in Relation to Cervical Dystonia” National Spasmodic Torticollis Association, Long Beach 2017
“Sleep Apnea, Co-morbidities & Treatment from the Dental Prospective” AAMS 12TH Annual Las Vegas, September 12TH, 2015
“Systemic Correlates of the Temporomandibular Joint” Power of Pain Conference, November 2014
“TMD: Clinical Implications and Interventions” UCLA Translational Science in Dentistry November 4, 2014
“TMJ Sequela” UCLA Oral Biology February 10, 2014
“TMJ Disorders” UCLA Oral Biology February 3, 2014
“TMJ” UCLA Oral Biology, January 27, 2014
11th Armenian Medical World Congress; Los Angeles, California July 2013 “Temporomandibular Joint Disease: Treatment with dental Orthopedics”
“Temporomandibular Joint Disorders, Orthopedics and Joint Disease Correlates to Systemic conditions”
“Arch Expansion and Mandibular Orthopedics for Pediatric Sleep Apnea”
AAAS-PD 94th Annual Meeting. “Patient –Centered Diagnosis and Therapies of Systemic Sequalae of Temporomandibular Joint Disease”; Las Vegas, Nevada: June 2013
“Systemic Correlates of the Temporomandibular Joint” Advanced Oral Biology Course, UCLA January 2013
“Systemic Correlates of the TMJ”; Power of Pain Conference, November 2012
“Temporomandibular Joint: a potential Treatment for Spasmodic Torticollis” NSTA Annual Symposium; New Orleans, Louisiana; October 2012
“Temporomandibular Joint”: Advanced Oral Biology Course, UCLA; January 2012
“Temporomandibular Joint; a potential treatment for Spasmodic Torticollis” NSTA Annual Symposium, Las Vegas, Nevada; October 2011
“TMJ Treatments and Systemic Correlates” ACI Study Club, Chino Hills; September 2011
AAAS-PD 92nd Annual Meeting “Systemic Correlate of the Temporomandibular Joint” San Diego; June 2011
“TMJ Treatments in Parkinson Patients”, Arcadia and Pasadena Parkinson Support Group; March 2011
“TMJ, Reticular Formation and Parkinson’s” Parkinson’s Resource Organization January 2011
“TMJ Treatments with Movement Disorder Patients”; UCLA Research Group November 15, 2010
“What to look for & do to avoid TMJ flare ups” Armenian Dental Society September 2010
“TMJ and Dystonia”, NSTA Annual Symposium, Baltimore, Maryland; September 2010
“TMJ and Arch Expansion in Children and Adults with Sleep Disorders”; Pomona Valley Hospital Sleep Panel, 2009
“TMJ”; Armenian Dental Society August 2008
Barkhordarian A, Demerjian G, Chiappelli F. Translational research of temporomandibular joint pathology: a preliminary biomarker and fMRI study. J Transl Med (2020) 18:22.
Demerjian GG et.al. (eds.), Temporomandibular Joint and Airway Disorders, Head and Neck Manifestations of Temporomandibular Joint Disorders. Springer Nature 2018.
Demerjian GG, Barkhordarian A, and Chiappelli F. Editors. “Temporomandibular Joint and Airway Disorders, A Translational Perspective” Springer Nature 2018. Gewerbestrasse 11, 6330 Cham, Switzerland.
Demerjian GG, Barkhordarian A, and Chiappelli F. “Neuroanatomy of the Trigeminal Nerve and Proximal Innervations of the TMJ.” Chapter 1, Pg. 3-15. Temporomandibular Joint and Airway Disorders, A Translational Perspective. Springer Nature 2018. Gewerbestrasse 11, 6330 Cham, Switzerland.
Barkhordarian A, and Chiappelli F, Demerjian GG. “Neuroanatomy and Neurophyiology of the Trigeminal Network System.” Chapter 2, Pg. 17-38. Temporomandibular Joint and Airway Disorders, A Translational Perspective. Springer Nature 2018. Gewerbestrasse 11, 6330 Cham, Switzerland.
Barkhordarian A, and Chiappelli F, Demerjian GG. “Neuroimmune and Systemic Manifestations of Neuroinflammation in the Temporomandibular Joint and Related Disorders.” Chapter 3, Pg. 39-60. Temporomandibular Joint and Airway Disorders, A Translational Perspective. Springer Nature 2018. Gewerbestrasse 11, 6330 Cham, Switzerland.
Demerjian GG, Sims AB, Patel M, Balatgek T, Sabal L. “Head & Neck Manifestations of Temporomandibular Joint Disorders.” Chapter 5, Pg. 73-93. Temporomandibular Joint and Airway Disorders, A Translational Perspective. Springer Nature 2018. Gewerbestrasse 11, 6330 Cham, Switzerland.
Sims AB, Demerjian GG. “Temporomandibular Joint Dysfunction, Trigeminal Nerve Inflammation, and Biomechanical Dental Treatments for the Suppression of Neurological and Neuropsychiatric Symptoms.” Chapter 6, Pg. 95-123. Temporomandibular Joint and Airway Disorders, A Translational Perspective. Springer Nature 2018. Gewerbestrasse 11, 6330 Cham, Switzerland.
Patel M, Demerjian GG, Sims AB. “The Relationship of Temporomandibular Joint, Orofacial Pain and Sleep Apnea.” Chapter 7, Pg. 125-134. Temporomandibular Joint and Airway Disorders, A Translational Perspective. Springer Nature 2018. Gewerbestrasse 11, 6330 Cham, Switzerland.
Demerjian GG, Pooja Goel. “Immunologic and Physiologic Effects of Dental Sleep Appliance Therapy.” Chapter 8, Pg. 135-171. Temporomandibular Joint and Airway Disorders, A Translational Perspective. Springer Nature 2018. Gewerbestrasse 11, 6330 Cham, Switzerland.
Balategel T, Demerjian GG, Sims AB, Patel M. “CBCT & MRI of Temporomandibular Joint Disorders and Related Structure.” Chapter 10, Pg. 201-217. Temporomandibular Joint and Airway Disorders, A Translational Perspective. Springer Nature 2018. Gewerbestrasse 11, 6330 Cham, Switzerland.
Chiappelli F, Barkhordarian A, Demerjian GG. “Patient-centered outcomes research and collaborative evidence-based medical and dental practice for patients with Temporomandibular Joint Disorders.” Chapter 11, Pg. 219-238. Temporomandibular Joint and Airway Disorders, A Translational Perspective. Springer Nature 2018. Gewerbestrasse 11, 6330 Cham, Switzerland.
Chiappelli F, Barkhordarian A, Demerjian GG. “Patient-centered outcomes research and collaborative evidence-based medical and dental practice for patients with Temporomandibular Joint Disorders.” Chapter 12, Pg. 239-249. Temporomandibular Joint and Airway Disorders, A Translational Perspective. Springer Nature 2018. Gewerbestrasse 11, 6330 Cham, Switzerland.
Demerjian GG, Barkhordarian A, and Chiappelli F. Testing patient targeted therapies in patients with temporomandibular joint disorder with the arthrokinetic reflex: individual patient research Journal of Translational Medicine 2016, 14:231.
Sims AB, Stack BC, Demerjian GG. Spasmodic Torticollis: The Dental Connection; Cranio Journal 2012, 30:188-93.
Barkhordarian A, Ajaj R, Ramchandani M, Demerjian G, Cayabyab R, Danaie S, Ghodousi N, Iyer N, Mahanian N, Phi L, Giroux A, Manfrini E, Neagos N, Siddiqui M, Cajulis O, Brant X, Shapshak P, Chiappelli F. Osteoimmunology in HIV/AIDS: A Translational Evidence-Based Perspective, Pathology Research International 2011, E. pub 2011 May 21.
Demerjian G, Sims A, Stack B. Proteomic Signature of Temporomandibular Joint Disorders(TMD): Toward diagnostically predictive biomarkers, BioInformation 2011, 5:282-4.
Barkhordarian A, Demerjian G, Jan A, Sama N, Nguyen M, Du A, Chiappelli F. Stakeholder engagement analysis - a bioethics dilemma in patient-targeted intervention: patients with temporomandibular joint disorders, J Transl Med. 2015; 13: 15.
Chiappelli F, Barkhordarian A., Demerjian G, Bach Q, Vandan Kasar. Cluster Randomized Stepped Wedge Blinded Controlled Trials (CRSWBCT) In Comparative Effectiveness Research (CER) – Part II: Implications for Temporomandibular Joint Disorders (TMD) Research, Transl Med (Sunnyvale) 2015, 5:3.
Chiappelli F, Barkhordarian A. Demerjian G, Bach Q, Vandan Kasar. Cluster Randomized Stepped Wedge Blinded Controlled Trials (CRSWBCT) In Comparative Effectiveness Research (CER) – Part I: Toward a Revision of CONSORT, Transl Med (Sunnyvale) 2015, 5:3.
Abstracts:
Demerjian G, Barkhordarian A, Sims AB, Chiappelli F. Systemic Correlates of TMJ Neuro-Inflammation. Systemic Correlates of TMJ Neuro-Inflammation (#105). World Dental Federation (Fédération dentaire internationale, FDI) Annual Dental Congress, Istanbul, Turkey, August 28-31, 2013.
Demerjian G, Barkhordarian A, Sims AB, Chiappelli F. Temporomandibular Joint Disorders Orthopedics and Joint Disease correlates to systemic conditions. 11th Armenian Medical World Congress, Hollywood, California, July 3-7, 2013.
Demerjian G, Sims AB, Barkhordarian A, Chiappelli F. Dental Arch Expansion and Mandibular Orthopedic Correction in Children: A Treatment for Pediatric Sleep Apnea. 11th Armenian Medical World Congress, Hollywood, California, July 3-7, 2013.
Demerjian G, Sims AB, Barkhordarian A, Chiappelli F. Temporomandibular Joint Disease: Treatment with Dental Orthopedics for Pain Management. 11th Armenian Medical World Congress, Hollywood, California, July 3-7, 2013.
Barkhordarian A, Demerjian G, Chiappelli F. Systemic correlates and local responses to Temporomandibular Joint Disorders. 94th AAAS-PD Annual Meeting, Las Vegas, NV; June 15-19, 2013.
Demerjian G. Patient- Centered Diagnosis and Therapies of Systemic Sequelae of Temporomandibular Joint Disorders. 94th AAAS-PD Annual Meeting, Las Vegas, NV; June 15-19, 2013.
Dr. Demerjian grew up in Pasadena and his family moved to La Verne in 1981. He has been practicing dentistry in the city of Glendora since 1990 and in the San Fernando Valley since 2001. He is an avid Martial Arts practitioner, holding several Black Belts in numerous styles. He serves as the head instructor for Marquez School of Hope, teaching karate to all students including to the specially challenged. He is on the Dental Advisory Committee at Citrus College and the Sleep Panel at the Pomona Valley Hospital. He maintains active membership in numerous scientific organizations.





 hover background
hover background hover background
hover background hover background
hover background hover background
hover background hover background
hover background hover background
hover background













 hover background
hover background 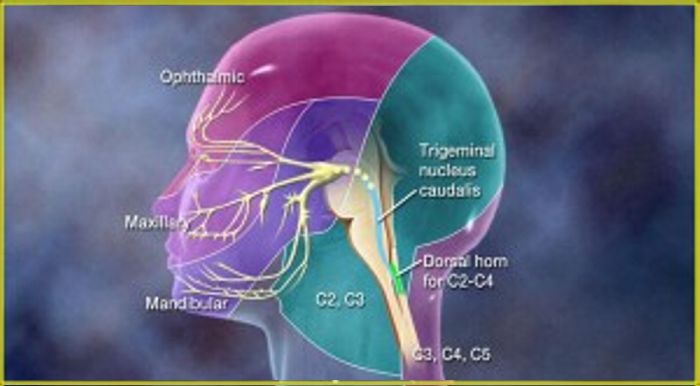 hover background
hover background  hover background
hover background
 hover background
hover background hover background
hover background hover background
hover background hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background hover background
hover background hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background
 hover background
hover background